Abstract
Introduction: Communicating about the risk of mortality after allogeneic hematopoietic stem cell transplantation (HCT) is a challenging task for physicians. This is especially true for elderly patients with aggressive hematologic malignancies. Mortality after HCT may be split in three major parts, death after relapse, therapy-related mortality (including late complications of previous treatments of the hematologic malignancies) and background or general population mortality from causes unrelated to the treatment or disease. In the framework of the competing endpoints, relapse and non-relapse mortality, background mortality mainly determines the magnitude of non-relapse mortality. To estimate the size of the background mortality, the risk of an age-, sex-, country- and calendar year matched population can be used as approximation. This can be done with methods from relative survival analysis. By nature, background mortality increases among elderly patients. In order to study the size of background and excess mortality we analyzed mortality in a population of adult transplant recipients with myelodysplastic syndromes (MDS) because this indication is characterized by a high median age already at diagnosis and large numbers of transplanted patients.
Patients and Methods: Data from adult patients with MDS who had received a first allogeneic HCT between January 2000 and December 2012, and who were registered with the EBMT database, were analyzed. Patients who had received mismatched related HCT or cord-blood transplantation were excluded from this analysis due to insufficient numbers of patients in the respective subgroups. For the statistical analysis we combined relative survival methods and multi-state modeling (Pohar M (2006) and de Wreede LC (2010), both in Computer Methods and Programs in Biomedicine). Outcomes were calculated since HCT. Outcomes of the subgroup of patients still alive and disease-free at 2 years after HCT were also analyzed to focus on the long-term prognosis of patients who had not suffered from early treatment failure.
Results: In total, 6434 patients were included into the analysis. The number of transplants increased from 185 in the year 2000 to 862 in 2012. Median age at alloHCT increased from 49 years (range 18 to 70 years) in 2000 to 58 years (18-76 years) in 2012 (Wilcoxon rank sum test, p<0.001). During the same period of time the number of patients who were 65 years or older at the time of alloHCT increased from 9 (5% of all patients transplanted in 2000) to 150 (17% of all patients transplanted in 2012).
The probability of overall survival (OS) decreased from 53% (95%CI, 52-55%) at two years to 43% (95%CI, 42-45%) at five years and to 35% (95%CI, 34-37%) at ten years after alloHCT. The 5-year survival probability calculated from the day of HCT was 53% (95%CI, 50-56%) for patients <45 years of age at alloHCT compared to 35% (95%CI, 32-39%) for patients above 65 years. Conversely, 5-year non-relapse mortality (NRM) was 25% (95%CI, 22-27%) and 36% (95%CI, 32-39%), for the respective age groups.
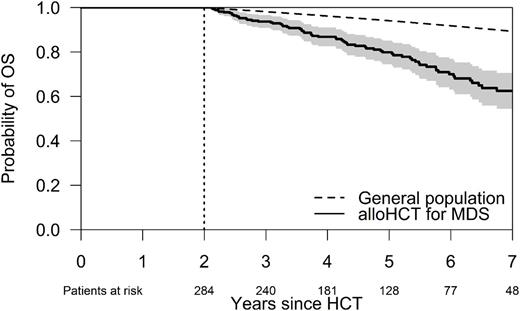
At the 2-year landmark (LM) 2578 patients in the dataset were alive and disease-free. The 5-year OS probability from this LM was 88% (95%CI, 86-91%) for patients <45 years of age at alloHCT compared to 63% (95%CI, 55-71%) for patients transplanted at an age ≥65 years. The figure below shows the probability of overall survival with associated 95%CIs for patients aged ≥65 years at alloHCT who were alive and disease-free at the 2-year LM compared to the survival of the general population matched to the patient population by age, sex, country and calendar year. The cumulative incidence of NRM during the same period was 7% (95%CI, 4-9%) for patients <45 years of age compared to 25% (95%CI, 18-32%) for patients transplanted at an age ≥65 years. Notably, of the 5-year NRM calculated for the 2-year LM population of patients who were transplanted at an age ≥65 years, 35% of deaths could be contributed to background mortality.
Conclusions: We show very favorable long-term outcomes after allogeneic HCT for patients with MDS. While long-term survivors of all age groups are at risk for excess mortality, the results of this study suggest that for elderly patients a substantial part of non-relapse mortality after HCT has to be attributed to background mortality. These results may help in communicating the risk of mortality after HCT especially for elderly patients in a more balanced way.
Schetelig: Sanofi Aventis: Consultancy, Research Funding; Roche: Honoraria; Abbvie: Honoraria; Janssen: Consultancy, Honoraria. Platzbecker: Acceleron: Consultancy, Honoraria, Research Funding; Celgene: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Research Funding; Janssen: Consultancy, Honoraria, Research Funding. Luft: Alexion: Consultancy; Neovii: Research Funding. Kobbe: Celgene: Other: Advisory Board, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal